Investing in Bariatric Benefits at the Workplace
By: Caitlin Kennington, Insurance Specialist
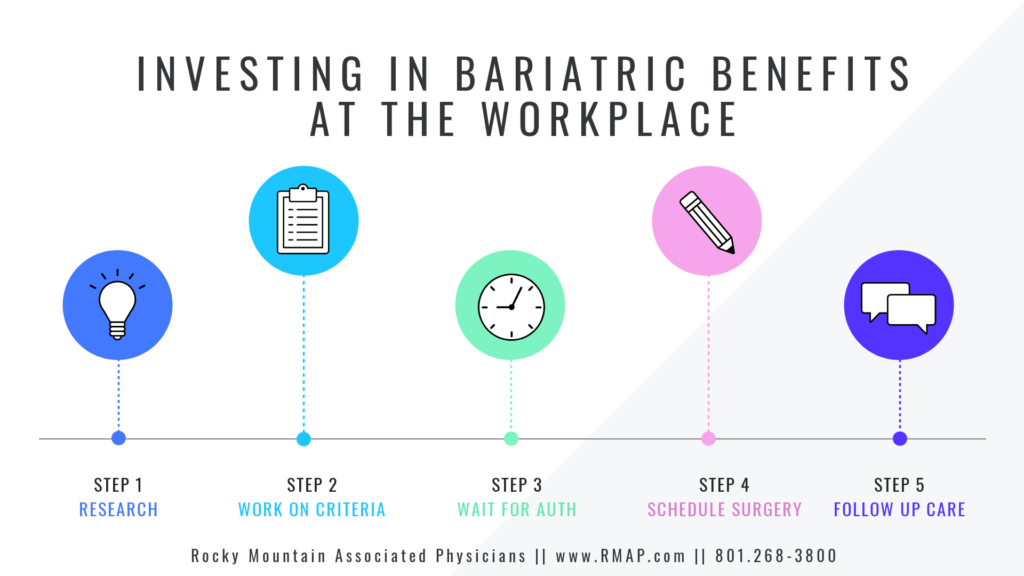
Learn more about weight loss surgery at Rocky Mountain Associated Physicians www.RMAP.com (801) 268-3800
In 2013, the American Medical Associated declared obesity a disease, which currently affects 41.9% of the United States population.1 All over the internet you will see ads for fitness programs, weight loss regimes, fad diets, fat-burning supplements, and prescription drugs all aimed at fighting the continual rise on the collective body mass index of consumers. However, when it comes to treating the morbidly obese, which is defined as those with a BMI of over 40, the only scientifically proven long-term effective and durable option is through metabolic and bariatric surgeries (weight loss surgery). These surgeries include the Gastric Bypass Roux-en-Y, Sleeve Gastrectomy, and the Biliopancreatic Diversion with Duodenal Switch.
Obesity is a disease that takes an emotional toll on those who suffer but also significantly impacts employers through increased health spending and in decreased productivity from less healthy employees. Due to these negative implications of obesity, more employer groups have begun recognizing the benefits of surgical weight loss and adding bariatric riders to their insurance plans. These riders are extremely effective additions to the policies as they allow access to more durable weight management options which cure and prevent obesity-related health conditions, which are very costly, and therefore provide a good financial investment. Additionally, surgery adds to better workplace productivity by increasing the number of healthy employees who are then more active and engaged in the workforce and are less likely to engage in medical-related absenteeism or require short-term or long-term disability.
Obesity, especially morbid obesity, is a very misunderstood disease with those who are affected being viewed as too lazy to stick to a healthy diet and exercise routine. Many employers feel that obesity in the workplace is a matter of a lack of lifestyle discipline.2 As such, their efforts to fight the rise in obesity have been focused solely on providing fitness facilities, incentivizing weight management programs, or providing healthier cafeteria options. However, despite these workplace efforts, the obesity rates in the country have continued to rise, growing 11.4% from 2000-2022.3 Obesity is more complex than calories in and calories burned, with a great number of metabolic factors contributing. It is in treating the metabolic factors that bariatric surgeries are so much more effective in creating a more effective and durable weight treatment option than just lifestyle modifications.
In a long-term study by the Swedish Government those who were on a monitored and controlled program of lifestyle modifications only lost 2% of their body weight or an average of 15 lbs. over a period of ten years.4 In contrast, the University of Utah found that those who had the Gastric Bypass surgery lost and maintained a 26.9% weight loss or an average of 80.2 lbs. in the 14 years following surgery.5 Employers who give the option of opting into bariatric surgery benefits, therefore, will find that those who do will find more long-term success.
Oftentimes, employers will cite cost as the primary factor in choosing not to offer bariatric surgery benefits. However, the belief that it is too expensive of an option to offer is based on a lack of understanding of the long-term effect surgery has on chronic conditions and the financial implications thereof. It has been found that bariatric surgery pays for itself within 2 years.6 The primary cause for such a quick return on investment can primarily be attributed to the effects that surgery can have on chronic and expensive medical conditions.
It is estimated that hypertension, osteoarthritis, chronic back pain, and Type 2 Diabetes cost $1.7 trillion per year, with 18% of the cost being attributed to Type 2 Diabetes alone.7 Per the CDC, Type 2 Diabetes affects roughly 35 million Americans. Bariatric surgery has a particularly strong and immediate effect on Type 2 Diabetes with reports of insulin resistance dropping between 34-51% depending on the surgery, within the first 1-2 weeks following surgery.8 In the long-term, at 2 years 75% of patients undergoing Gastric Bypass found their diabetes in remission. At 6 years 65% of patients remained in remission, and at 12 years 51% of patients had maintained the remission of their diabetes.9
Because the treatment for and economic impact of Type 2 Diabetes is so high, the resulting remissions from surgery account for significant health cost savings. This estimates the huge impact of just one medical condition. Indeed, the cost benefits will only increase as inflation and exorbitant mark-ups on medication continue to drive the price up for treatment. Surgery has also been shown beneficial in treating hypertension, sleep apnea, hyperlipidemia, and Non-Alcoholic Steatohepatitis, as well as preventing obesity-related cancers and degenerative joint disease.
With all the costs associated with these conditions, obesity is estimated to cost $1.39 trillion per year in medical expenses, making it a wise financial decision to invest funds into paying for addition bariatric surgery riders on employer-provided group health plans.10
Finally, investing in the bariatric benefit allows patients to access care that will give them years of improved health, which is more likely to keep these employees in the workforce by reducing absenteeism, worker’s compensation claims, and short-term and long-term disability. Obesity is hard on the body, which results in more physical limitations, more musculoskeletal injuries, decreased mobility, and longer healing times from injuries. All these factors contribute to decreased productivity, and more requested leave being taken medical concerns.
Indeed, obese workers have been found to have a higher number of missed workdays, lower productivity, and a 76% higher rate of short-term disability claims.11 Additionally, obese workers are more likely to leave the workforce entirely due to medical concerns associated with obesity. Those who are obese make up 43% of new Social Security Disability applications, while those in a healthy BMI range made up 23%.12 All-in-all, healthier employees are more engaged, more present, and more effective employees and weight is a significant factor negatively impacting the workforce.
Obesity is a hugely impactful issue with the effects being widespread and detrimental. Many employer groups have recognized the benefits of encouraging weight loss in their employees; however, it is those who recognize the durability and effectiveness of bariatric surgeries who are more likely to see their employees lose more weight and maintain their weight loss. Those same employers who add the bariatric surgery rider will also find that as employees take advantage of the option, they will lower their health insurance costs. Finally, they will also see more employees maintain their health and stay engaged and productive in the workforce.
In conclusion, due to the overall positive impact these surgeries have for both the employer and the employee, these insurance riders are extremely beneficial and an effective tool in battling the obesity epidemic.
About the Author:

Caitlin is one of Rocky Mountain Associated Physicians (RMAP)’s insurance specialist by verifying patient’s insurance coverage and helping them with insurance criteria benefits. She was raised in Brigham City, Utah and Las Vegas, Nevada along with five of her siblings. She studied Art History at the University of Utah and is a Certified Gemologist and Jeweler. Caitlin enjoys reading, making jewelry, and spending time with her family, especially her husband, son and daughter.
Links to related articles:
Weight Loss Surgery and the Insurance Process
Preparing Emotionally for Bariatric Surgery
Type 2 Diabetes and Bariatric Surgery
www.RMAP.com
Rocky Mountain Associated Physicians
801-268-3800
1160 East 3900 South, Suite 4100
SLC, UT 84124
Resources
- Centers for Disease Control and Prevention. (2022, May 17). Adult obesity facts. Centers for Disease Control and Prevention. Retrieved November 25, 2022, from https://www.cdc.gov/obesity/data/adult.html
- Gabel, J. R., Whitmore, H., Pickreign, J., Ferguson, C. C., Jain, A., KC, S., & Scherer, H. (2009). Obesity and the workplace: Current programs and attitudes among employers and employees. Health Affairs, 28(1), 46–56. https://doi.org/10.1377/hlthaff.28.1.46
- Centers for Disease Control and Prevention. (2022, May 17). Adult obesity facts. Centers for Disease Control and Prevention. Retrieved November 25, 2022, from https://www.cdc.gov/obesity/data/adult.html
- Sjöström, L. (2013). Review of the key results from the Swedish obese subjects (SOS) trial – A prospective controlled intervention study of bariatric surgery. Journal of Internal Medicine, 273(3), 219–234. https://doi.org/10.1111/joim.12012
- Adams, T. D., Davidson, L. E., Litwin, S. E., Kim, J., Kolotkin, R. L., Nanjee, M. N., Gutierrez, J. M., Frogley, S. J., Ibele, A. R., Brinton, E. A., Hopkins, P. N., McKinlay, R., Simper, S. C., & Hunt, S. C. (2017). Weight and metabolic outcomes 12 years after Gastric Bypass. New England Journal of Medicine, 377(12), 1143–1155. https://doi.org/10.1056/nejmoa1700459
- Cremieux PY, Buchwald H, Shikora SA, Ghosh A, Yang HE, Buessing M. A study on the economic impact of bariatric surgery. Am J Manag Care. 2008 Sep;14(9):589-96. PMID: 18778174.
- Weighing down America: 2020 update. Weighing Down America: 2020 Update. (n.d.). Retrieved November 25, 2022, from https://milkeninstitute.org/report/weighing-down-america-2020-update
- Rao, R. S., Yanagisawa, R., & Kini, S. (2011). Insulin resistance and bariatric surgery. Obesity Reviews, 13(4), 316–328. https://doi.org/10.1111/j.1467-789x.2011.00955.x
- Adams, T. D., Davidson, L. E., Litwin, S. E., Kim, J., Kolotkin, R. L., Nanjee, M. N., Gutierrez, J. M., Frogley, S. J., Ibele, A. R., Brinton, E. A., Hopkins, P. N., McKinlay, R., Simper, S. C., & Hunt, S. C. (2017). Weight and metabolic outcomes 12 years after Gastric Bypass. New England Journal of Medicine, 377(12), 1143–1155. https://doi.org/10.1056/nejmoa1700459
- Weighing down America: 2020 update. Weighing Down America: 2020 Update. (n.d.). Retrieved November 25, 2022, from https://milkeninstitute.org/report/weighing-down-america-2020-update
- Dor, A., Ferguson, C., Langwith, C., & Tan, E. (2010, September 21). A heavy burden: The individual costs of being overweight and obese in … GW Himmelfarb Health Sciences Library. Retrieved November 25, 2022, from https://publichealth.gwu.edu/departments/healthpolicy/DHP_Publications/pub_uploads/dhpPublication_35308C47-5056-9D20-3DB157B39AC53093.pdf
- Hyde, J. S. (2016, January 30). The Prevalence of Obesity Among Recent Applicants to Federal Disability Programs. Washington, DC: Center for Studying Disability Policy, Mathematica Policy Research. Retrieved November 25, 2022, from https://www.mathematica.org/publications/the-prevalence-of-obesity-among-recent-applicants-to-federal-disability-programs.

















 Address: 1521 East 3900 South STE 100
Address: 1521 East 3900 South STE 100 Office: +
Office: +  Fax number (801) 268-3997
Fax number (801) 268-3997 Email: info@rmapinc.com
Email: info@rmapinc.com



