Learn more about weight loss surgery at Rocky Mountain Associated Physicians www.RMAP.com (801) 268-3800
It is well known that losing weight—or regain after bariatric surgery—is hard. Keeping weight off and maintaining can be just as challenging. There are few studies out there in the medical community still trying to straighten out the connections between sleep and weight, but there are some which emphasize the potential weight loss benefits of a good night’s sleep and negative health impacts of sleep deprivation.
New research suggests that adults who are better rested consume significantly fewer calories than those who are chronically sleep-deprived. A study published by JAMA Internal Medicine finds that people who sleep less consume more calories and foods that are high in calories. This is compared with people who sleep for longer periods.1
The study concludes with the participants who slept an hour longer each night consumed an average of 270 fewer calories each day and lost about a pound compared to control group participants, who gained just under a pound on average.
The Link Between the Stomach and Your Appetite
True or false: Your appetite is linked to your stomach. Answer: False. Your appetite is actually controlled by the neurotransmitter’s ghrelin and leptin, not your stomach. The hormone ghrelin promotes hunger and increases appetite. The hormone leptin contributes to the sensation of feeling full. The body will naturally increase and decrease the levels of these neurotransmitters throughout the day, signaling the need to consume calories.2
Obesity and Sleep Deprivation
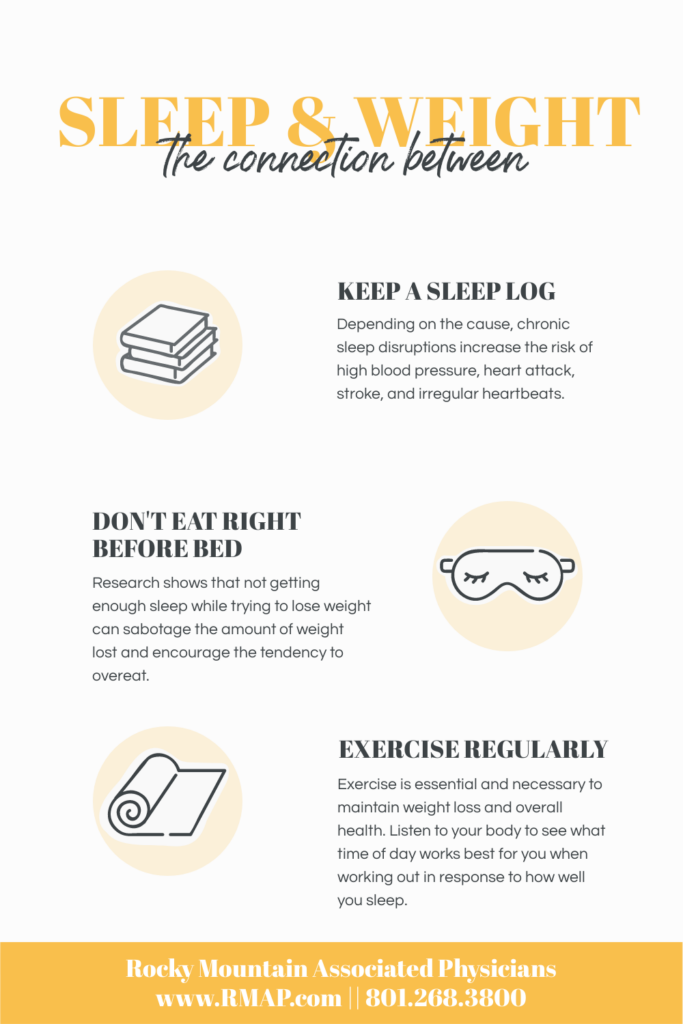
Depending on the cause, chronic sleep disruptions increase the risk of high blood pressure, heart attack, stroke, and irregular heartbeats.3
Past studies show that people who get less than 6 hours of sleep at night are more likely to be diagnosed as obese, though it’s difficult for these studies to determine cause and effect.4 Obesity in itself can cause an increase risk of developing conditions that interfere with sleep, such as sleep apnea. Though it’s unclear if not getting enough sleep is the cause of obesity, and/or if obesity is causing people to sleep less. Commonly, sleep-deprived individuals tend to choose foods that are high in calories and carbohydrates.5
Sleep and Losing Weight
Research shows that not getting enough sleep while trying to lose weight can sabotage the amount of weight lost and encourage the tendency to overeat.6 When treating obesity in adults, medical experts encourage improving sleep quality.
Sleep and Physical Activity
When you aren’t getting enough sleep, it can result in having less energy for exercise and physical activity. Exercise is essential and necessary to maintain weight loss and overall health. For example: walking, running, weightlifting, dancing, swimming, sports, etc. Listen to your body to see what time of day works best for you when working out in response to how well you sleep. For some individuals, exercising too late in the day can interfere with how well they rest at night.
Ways to Help Improve Sleep
It’s important to try and get adequate sleep, as well as quality sleep, as part of a healthy weight plan. Here we have put together some tips and suggestions that could help improve your sleep:
- Keep to a regular sleep schedule
- Sleep in a dark room; purchasing blackout curtains can help with blocking out light and noise
- Don’t eat right before bed
- Reduce stress
- Become an early bird
- Keep a sleep log
- Monitor sleep times with wrist actigraphy devises such as smartwatches
- Limit use of electronic devises at least 1 hour before bed
- Turn temperature to a comfortable number
- Exercise regularly
Healthy Looks Different for Everyone
Remember that good health and healthy looks and feels different for everyone. Health is a lifelong journey that includes not only healthy habits and eating nutritious foods, but by also having a healthy relationship with your body. Work closely with your doctor’s guidance, as well as keeping your own personal decisions in mind.
Links to related articles:
The Negativity of Weight Stigma and Bias
Changing Old Behaviors
Why Am I Always so Tired?
Tips for a Lifestyle of Healthy Nutrition
www.RMAP.com
Rocky Mountain Associated Physicians
801-268-3800
1160 East 3900 South, Suite 4100
SLC, UT 84124
Resources
- Esra Tasali, MD, Kristen Wroblewski, MS, Eva Kahn, MS, et al Jennifer Kilkus, MS, RDN, Dale A. Schoeller, PhD, “Effect of Sleep Extension on Objectively Assessed Energy Intake Among Adults with Overweight in Real-life Settings”, JAMA Intern Med., 2022; 182(4):365-374. Doi:10.1001/jamainternmed.2021.8098, https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2788694
- Karine Spiegel, Esra Tasali, Plamen Penev, Eve Van Cauter, “Brief Communication: Sleep Curtailment in Healthy Young Men is Associated with Decreased Leptin Levels, Elevated Ghrelin Levels, and Increased Hunger and Appetite”, Ann Intern Med., 2004 Dec 7; 141(11):846-50, doi: 10.7326/0003-4819-141-11-200412070-00008, https://pubmed.ncbi.nlm.nih.gov/15583226/
- “Losing Weight, Especially in the Belly, Improves Sleep Quality, According to a John Hopkins Study”, https://www.hopkinsmedicine.org/news/media/releases/losing_weight_especially_in_the_belly_improves_sleep_quality_according_to_a_johns_hopkins_study
- Yili Wu, Long Zhai, Dongfeng Zhang, “Sleep Duration and Obesity Among Adults: A Meta-analysis of Prospective Studies”, Sleep Med, 2014 Dec; 15 (12):1256-62, doi: 10.1016/j.sleep.2014.07.018, https://pubmed.ncbi.nlm.nih.gov/25450058/
- Stephanie M Greer, Andrea N Goldstein, Matthew P Walker, “The Impact of Sleep Deprivation on Food Desire in the Human Brain”, Nat Commun, 2013;4:2259, doi: 10.1038/ncomms3259, https://pubmed.ncbi.nlm.nih.gov/23922121/
- Marie-Pierre St-Onge, Andrew McReynolds, Zalak B Trivedi, Amy L Roberts, Melissa Sy, Joy Hirsch, “Sleep Restriction Leads to Increased Activation of Brain Regions Sensitive to Food Stimuli”, Am J Clin Nutr, 2012 Apr;95(4):818-24, doi: 10.3945/ajcn.111.027383, https://pubmed.ncbi.nlm.nih.gov/22357722/











 Address: 1521 East 3900 South STE 100
Address: 1521 East 3900 South STE 100 Office: +
Office: +  Fax number (801) 268-3997
Fax number (801) 268-3997 Email: info@rmapinc.com
Email: info@rmapinc.com



