Learn more about weight loss surgery at Rocky Mountain Associated Physicians || www.RMAP.com || (801) 268-3800
Bariatric surgery is a life-changing procedure, a powerful tool to achieve significant weight loss and improve overall health. However, it’s important to acknowledge that the journey doesn’t end with the surgery itself. Life changes, circumstances shift, and sometimes, weight regain becomes a reality several years post-surgery. Through 20 years of bariatric surgery practice, I have observed that significant challenging life events can often be linked to weight regain. These challenges may include a job change, a death in the family (or significant loss of any kind), a car accident, or any event that limits physical abilities. This article aims to guide individuals through the process of reclaiming control over their weight and fostering a healthier lifestyle after facing setbacks.
Understanding Weight Regain
Weight regain after bariatric surgery is not uncommon, and there are various factors that contribute to this challenge. These factors include metabolic changes, lifestyle choices, psychological factors, and hormonal fluctuations. In fact, it’s good to remember that some amount of weight gain reaching one’s lowest weight after surgery is actually normal. If you recall from our pre-operative classes, we review the normal weight loss trajectory following bariatric surgery.
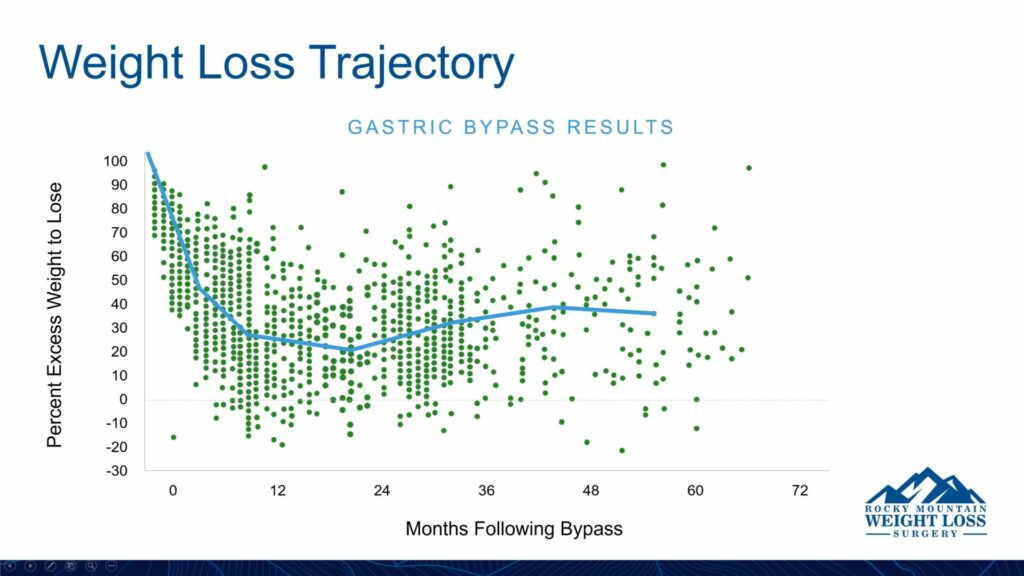
Most people reach their lowest weight 1-2 years after surgery and then re-gain about 15-20% of the weight they lost over the next 2-4 years. Beyond 6 years from surgery, our research indicates that the average weight loss across thousands of patients remains relatively stable, but individual variation definitely occurs. Life throws us curveballs–like the stressful events just mentioned—and they can happen at any time postoperatively. It’s crucial to approach weight regain with compassion and a willingness to explore the root causes before embarking on a new weight loss journey.
Reassessing Dietary Habits
One of the fundamental aspects of post-bariatric weight loss is reassessing and adapting dietary habits. After surgery, the stomach size is reduced, and certain foods may become difficult to tolerate. The inability to tolerate certain foods may be due to dumping syndrome, texture of the food, or simply a loss of appetite or “craving” that food. For foods that are high in sugar or carbs, this is a good thing as it promotes weight loss and aversion to these less nutrient dense foods.
However, over time, your body’s hormones may adapt, your gastric pouch or sleeve may often soften to allow a greater amount and variety of food to pass through, and old habits can creep back in. A good way to begin is by consulting with a registered dietitian or nutritionist to create a personalized meal plan that aligns with your surgery and addresses your specific nutritional needs. Those types of visits can be arranged through our office with Juliana (dietitian) or one of our nurse practitioners: Lissa Hutchings, Stacy Parry, or Elizabeth Hanna, who can help get you back on track. If you still have your blue binder, aka the “RMAP bible”, refer to it again to revisit early dietary instructions to help get started.
Focus on Protein Intake
Protein is a vital component for post-bariatric patients, as it supports muscle preservation and helps with satiety. Reevaluate your protein intake and ensure that it meets the recommended levels. We typically advise that during the first year after surgery, about 70% of your meal should be protein based. After the first year or achieving your weight loss goal, at least 50% of your meal should be protein based, but there is no harm in continuing the 70% protein level. Obtaining at least 1 gm of protein per kilogram (or 2.2 pounds) of body weight is a good goal. Include lean sources of protein such as poultry, fish, tofu, and legumes in your meals. Protein supplements may also be considered, but it’s essential to consult with healthcare professionals before incorporating them into your routine. We prefer wholesome naturally occurring protein foods, but protein shakes or supplements may be used if protein intake is otherwise very challenging.
Mindful Eating Practices
Practicing mindfulness during meals can significantly impact your relationship with food. Slow down, savor each bite, and pay attention to your body’s hunger and fullness cues. Avoid distractions like watching TV or using electronic devices while eating. This approach fosters a greater awareness of portion sizes and helps prevent overeating. Before eating, especially snacking, ask yourself, “Am I truly hungry?” Sometimes the answer will be “no”. If that’s the case, put off eating until a normal meal time or you are actually hungry. Try drinking water instead of eating. If you truly are hungry and you’re between meals, have a healthy protein-based snack available like a piece of string cheese, handful of nuts, or beef jerky.
Recommitting to Physical Activity
Regular physical activity is a key component of maintaining weight loss and overall well-being. Engage in activities that you enjoy and that align with your fitness level. Begin gradually and aim for a mix of cardiovascular exercises and strength training. We typically recommend aiming for 3 hours a week of physical activity. This may include a brisk walk, a jog or run, swimming, or cycling for cardiovascular activity, and strengthening activities like pushups, sit-ups, yoga, or lifting weights. Key features of your exercise routine are sustainability and consistency, so choose activities that you LIKE to do.
Seeking Emotional Support
Weight loss journeys are not solely physical; they also involve emotional and psychological components. It’s essential to address any emotional triggers or challenges that may contribute to weight regain. Consider seeking support from a mental health professional, joining a support group, or connecting with individuals who have undergone similar experiences. Our support groups at Rocky Mountain Associated Physicians offer a good starting point, and participation is free to those who have had surgery with us. Our patients also may seek individual counseling/therapy for a deeper dive into psychological triggers and solutions. Emotional well-being is integral to sustained weight loss success.
Role of Weight Loss Medications
As many people are aware, the FDA has recently approved more powerful weight loss medications such as semaglutide (Ozempic, Wegovy), and tirzepatide (Mounjaro, Zepbound). These drugs target a digestive hormone called glucagon-like polypeptide (GLP-1) that plays a key role in metabolism and weight control. Ozempic and Mounjaro are approved by the FDA for type 2 diabetes, but they have been used off-label for weight loss by some health care providers. The FDA recently approved these drugs under different brand names (Wegovy and Zepbound) specifically for weight loss. These medications may be costly depending on insurance coverage and/or in short supply, and they may have side effects such as nausea and vomiting. Nevertheless, they may be very helpful tools in helping patients re-lose weight after regain following bariatric surgery, especially in cases where earnest dietary and exercise changes have been consistent. We have two providers in the office, Stacy Parry and Elizabeth Hanna, who are available to see patients for medical weight loss after bariatric surgery.
When to Consider Revision Bariatric Surgery
This article primarily aims to address accessible and low-risk ways to reduce weight after regain following bariatric surgeries. Indeed, most patients are not anxious to have a second or third procedure for weight loss. With that said, revision bariatric surgery may be a reasonable option for some patients, including those whose BMI is above 40, or for those who may have (re)developed a major weight related problem, such as type 2 diabetes, high blood pressure, obstructive sleep apnea, or high cholesterol, despite maximizing efforts at diet, exercise, psychological health and medications.
At our practice, about 80% of our surgeries are primary bariatric surgeries, and 20% are revision surgeries. It is important to bear in mind that revision bariatric surgery typically involves more risk and less predictable benefits than primary weight loss surgery, which is why we encourage our patients to address diet, exercise, psychological health, and medications before seeking revision bariatric surgery for weight gain. Nevertheless, in some cases, it may be favorable to add metabolic power to a previous bariatric procedure through revision bariatric surgery.
For example, a gastric band can be removed and converted to a Sleeve, Gastric Bypass, or Duodenal Switch. A Sleeve can be converted to a Gastric Bypass—especially if severe reflux is a problem—or more commonly to a Duodenal Switch, which is a more powerful option to address significant weight gain after Sleeve. Finally, a Gastric Bypass can be converted to a Duodenal Switch, which is a more complex revision surgery. For complex revisions, we typically spend extra time going over risks and benefits to make a sound decision about whether benefits of revision surgery outweigh risks. Some insurance plans do not cover revision bariatric surgery for weight gain, so you may need to check with your plan or with our office to determine your insurance benefit.
Conclusion
Embarking on a weight loss journey after experiencing setbacks post-bariatric surgery requires a holistic approach that encompasses nutrition, physical activity, and emotion well-being. Remeber that each individual’s journey is unique, and there is no one-size-fits-all solution. Approach the process with patience and resilience. As a practice, we are here to provide support as you tackle this challenge. With commitment and the right strategies in place, it is possible to regain control of your weight and rediscover success on your post-bariatric journey.
About the Author:
 Dr. Rodrick D. McKinlay, MD, FACS, joined Rocky Mountain Associated Physicians (RMAP) in 2004 as a board-certified surgeon with expertise in minimally invasive or laparoscopic surgery. In addition to the surgical treatment of obesity, his practice involved a wide range of minimally invasive gastrointestinal surgery, including hernia repair, gallbladder removal, anti-reflux surgery, and the surgical treatment of the spleen and adrenal disorders.
Dr. Rodrick D. McKinlay, MD, FACS, joined Rocky Mountain Associated Physicians (RMAP) in 2004 as a board-certified surgeon with expertise in minimally invasive or laparoscopic surgery. In addition to the surgical treatment of obesity, his practice involved a wide range of minimally invasive gastrointestinal surgery, including hernia repair, gallbladder removal, anti-reflux surgery, and the surgical treatment of the spleen and adrenal disorders.
Links to related articles:
Habits Sabotaging Weight Loss
Overeating Triggers and Tips
Weight Regain: Living with Fear and Dread
www.RMAP.com
Rocky Mountain Associated Physicians
801-268-3800
1160 East 3900 South, Suite 4100
SLC, UT 84124











 Address: 1521 East 3900 South STE 100
Address: 1521 East 3900 South STE 100 Office: +
Office: +  Fax number (801) 268-3997
Fax number (801) 268-3997 Email: info@rmapinc.com
Email: info@rmapinc.com



